Fungal infections pose a considerable challenge in dermatological practice, leading to discomfort, esthetic concerns, and occasionally significant morbidity. The treatment landscape for such infections typically includes over-the-counter (OTC) antifungal creams and prescription-strength formulations. This article delves into the distinctions between these two categories of therapy, elucidating their efficacy, appropriateness for various conditions, pharmacodynamics, and therapeutic strategies.
Understanding the pharmacological landscape of antifungal agents is crucial for effective management. The primary distinction between prescription and OTC antifungal creams lies in their potency, indications, and the complexity of the underlying fungal infection they aim to treat. Familiarity with these disparities can empower patients and caregivers to make informed choices regarding their dermatological health.
The Nature of Fungal Infections
Fungal infections can range from innocuous superficial conditions such as athlete’s foot and ringworm to more severe systemic infections in immunocompromised individuals. The causative organisms include dermatophytes, yeasts, and non-dermatophyte molds, each possessing distinct pathogenic mechanisms and susceptibilities to antifungal agents. The superficial nature of many dermatophyte infections often leads to their initial management with OTC agents, rendering them appealing for widespread use. However, the extent and severity of the infection should guide treatment selection, making it essential to differentiate between minor infections and those that may warrant more aggressive intervention.
The Mechanisms of Action: Understanding Antifungal Agents
Antifungal agents exhibit various mechanisms of action, crucial in determining their therapeutic applications. The majority of OTC antifungal creams contain active ingredients such as clotrimazole, miconazole, and tolnaftate, which inhibit fungal cell membrane synthesis or disrupt energy metabolism. These agents are often effective for localized, superficial infections, providing a potent yet accessible treatment option for consumers.
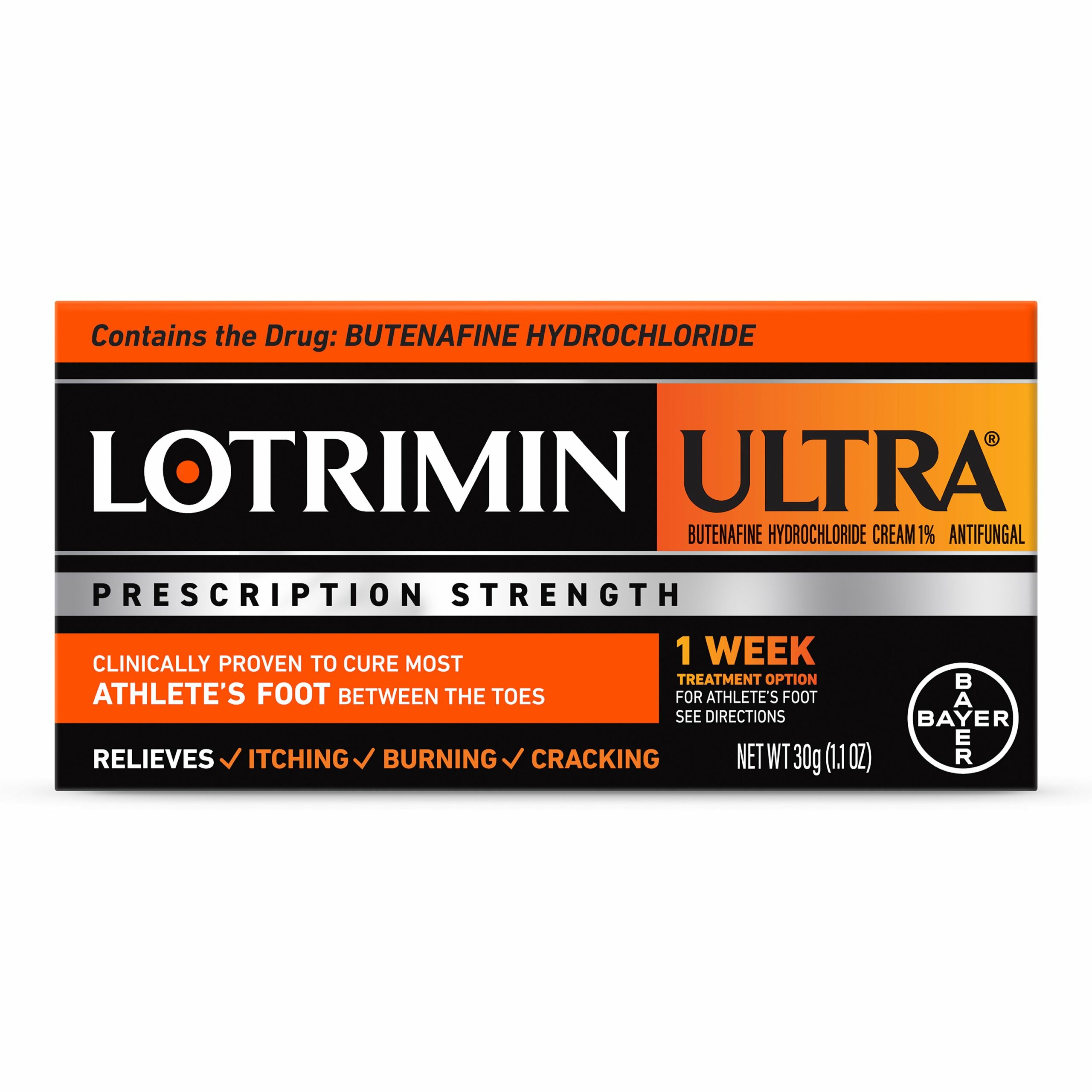
In contrast, prescription antifungal creams typically encompass stronger active ingredients, including but not limited to, butenafine, terbinafine, and prescription-only formulations tailored for specific conditions. These creams exert a more pronounced antifungal effect, targeting the fungal cell wall integrity, and thus are particularly beneficial for more complicated or refractory fungal infections. The pharmacokinetics and higher concentration of prescription formulations frequently translate into more rapid clinical improvement and enhanced outcomes in persistent cases.
OTC Antifungal Creams: Accessibility and Limitations
OTC antifungal creams offer a convenient solution for individuals seeking immediate relief from mild maladies. They are widely available and require no formal prescription, akin to other over-the-counter products such as analgesics or antihistamines. Commonly, these topical agents are indicated for dermatologic conditions characterized by superficial mycoses, including tinea pedis (athlete’s foot), tinea corporis (ringworm), and candidiasis.
Despite their availability, several limitations accompany OTC antifungal products. The primary concern is that they may not adequately address more severe infections, leading to persistent symptoms, complications, and potential progression of disease. Moreover, the lack of professional oversight can result in misdiagnosis, where individuals might self-treat a fungal infection without correctly identifying the underlying cause. This lapse in appropriate care could delay the initiation of necessary prescription treatments.
Prescription Antifungal Creams: The Gold Standard in Complex Cases
The cornerstone of antifungal therapy often hinges on prescription-strength formulations when dealing with challenging presentations. Healthcare professionals must evaluate the infection’s etiology, patient comorbidities, and drug contraindications before prescribing therapy. This meticulous assessment ensures a targeted therapeutic approach that optimizes patient outcomes while minimizing potential adverse effects.
Prescription antifungal creams are particularly adept at addressing recalcitrant infections, often incorporating systemic therapy in conjunction with topical application. For instance, when a localized infection is identified, such as onychomycosis (fungal nail infection), a combination of oral antifungals and topical creams may yield better results than topical agents alone. Similarly, prescription products can be formulated specifically for conditions like eczema or psoriasis complicated by fungal infections, providing tailored treatment for multifaceted dermatological issues.
Choosing Between OTC and Prescription: Factors to Consider
When navigating the decision between OTC and prescription antifungal creams, several factors warrant consideration. The severity, location, and type of fungal infection are paramount determinants. For instance, a mild case of athlete’s foot may respond favorably to OTC interventions, while an extensive or recurrent infection may necessitate a prescription product.
Additionally, patient demographics including age, underlying health conditions, and potential drug interactions play an essential role. Immunocompromised patients with underlying conditions such as diabetes or those taking immunosuppressive medications may require more comprehensive antifungal strategies due to their higher risk of severe infections and complications. Engaging in a dialogue with healthcare professionals can elucidate the most appropriate treatment pathway tailored to individual needs.
Evaluating Efficacy: Clinical Outcomes of Both Treatments
Clinical trials have scrutinized the efficacy of various antifungal treatments, highlighting both the strengths and limitations of OTC and prescription treatments. Meta-analyses have consistently demonstrated that while OTC antifungal creams provide adequate relief for mild infections, the performance of prescription formulations surpasses that of their OTC counterparts in terms of speed of recovery and long-term success rates, especially in complicated or chronic cases.
Moreover, patient adherence to therapy can influence clinical outcomes significantly. OTC treatments may contribute to improved compliance due to ease of access; however, many patients may not adhere to recommended treatment durations, undermining therapeutic success. Conversely, prescription therapies often come with professional guidance, enhancing adherence through better understanding of treatment rationales and regimen optimization.
The Future of Antifungal Therapy: Innovations on the Horizon
Antifungal therapy is on the cusp of notable innovations propelled by advances in pharmacology and a deeper understanding of fungal pathogens. Emerging agents and combination therapies are currently under investigation, promising enhanced efficacy and reduced resistance. Consequently, healthcare providers are urged to remain vigilant in keeping abreast of updated guidelines and evidence-based practices for fungal infection management.
Furthermore, the rise of telemedicine has facilitated consultations that allow for timely evaluation and management of fungal infections, ultimately bridging the gap between OTC accessibility and prescription interventions. Technological advancements in diagnostic methodologies can also assist in precise pathogen identification, thereby directing appropriate treatment from the outset and reducing unnecessary delays in care.
In conclusion, the decision to utilize OTC versus prescription antifungal creams is contingent upon various factors relating to the infection’s characteristics, patient demographics, and efficacy considerations. While OTC options provide a convenient pathway for managing mild ailments, prescription-strength medications remain the standard-of-care for complex fungal infections. A thorough understanding of the nuances and potential outcomes associated with each type of treatment will aid in making informed decisions that prioritize optimal patient health and wellness across the continuum of care.