Fungal infections pose a significant health concern, especially in humid climates where the favorable conditions for fungal growth prevail. This article delves into the most common fungal infections associated with high humidity levels and provides insightful perspectives on prevention and treatment options.
The interplay of humidity, temperature, and environmental factors catalyzes the proliferation of various fungi. As healthcare practitioners and enthusiasts alike, understanding these infections equips us with the necessary knowledge to combat their ramifications effectively.
Humidity is an omnipresent characteristic of tropical and subtropical regions, creating microenvironments conducive to fungal survival and replication. These environments, teeming with moisture, become breeding grounds for pathogens that can lead to infections in humans. The growing awareness of these conditions prompts us to challenge our current understanding and operational strategies in dealing with these infections.
Broadly, fungal infections can be categorized as superficial, subcutaneous, and systemic, with the focus here primarily on superficial infections commonly encountered in humid climates. These infections typically afflict the skin and mucous membranes and are often characterized by their vasculature and location-specific manifestations.
One can imagine a world teeming with inhospitable fungi lurking in every nook and cranny, waiting to take advantage of the unwary. With this vivid imagery, we embark on a journey through the most prevalent fungal infections that challenge public health in humid regions.
Common Fungal Infections in Humid Climates
While a multitude of fungal pathogens exists, three infections routinely emerge as the foremost concerns in warm, damp environments: tinea infections, candidiasis, and fungal nail infections. Distinct in their clinical presentations and causative agents, each warrants detailed exploration.
Tinea: The Ringworm Resurgence
Tinea, or ringworm, refers to a group of dermatophyte infections caused by fungi that invade keratinized tissues such as skin, hair, and nails. It is critical to note that the term “ringworm” is somewhat of a misnomer, as it is not caused by a worm but rather fungal entities from the genera Trichophyton, Microsporum, and Epidermophyton.
Within humid climates, tinea is notably prevalent and manifests as various clinical forms, such as tinea pedis (athlete’s foot), tinea cruris (jock itch), and tinea corporis (body ringworm). Tinea pedis, in particular, can exacerbate during summer months when individuals frequently don closed shoes, trapping moisture and heat, creating an inviting environment for fungal colonization.
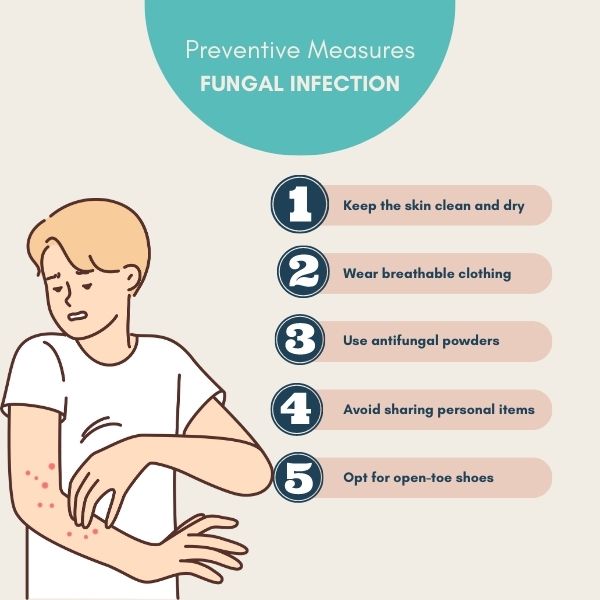
Symptoms often include the quintessential itchy, red, and scaly rash. Patients may also experience discomfort and lesions that can lead to secondary bacterial infections if left untreated. The transmission of tinea occurs primarily through direct skin-to-skin contact or indirectly via contaminated surfaces such as locker room floors and communal showers. The challenge, therefore, lies in both education and prevention, as effective measures include maintaining skin hygiene, wearing breathable footwear, and limiting exposure to communal wet areas.
Candidiasis: Fungal Overgrowth and Its Implications
Candida species, particularly Candida albicans, are resident microorganisms found within the human microbiome. However, in humid climates, the balance may tip in favor of this opportunistic fungus, resulting in candidiasis. When immunocompromised or subjected to certain risk factors, individuals may experience localized or systemic candidal infections, often characterized by inflammation, discomfort, and, in some cases, systemic illness.
Oral thrush and vaginal candidiasis are the most commonly encountered forms, manifesting as white lesions in the mouth or genital discomfort, respectively. It is intriguing to consider how environmental conditions that promote high humidity can foster the persistence of these infections, calling for vigilance in community health practices.
Risk factors associated with candidiasis comprise the use of broad-spectrum antibiotics, immunosuppression, diabetes, and poor dietary habits. Addressing these underlying issues is paramount in combating the candidal menace. The challenge lies not only in treating symptomatic infections but also in adopting preventive strategies that bolster immune defenses, such as dietary modifications, enhanced oral hygiene, and moisture control in susceptible areas.
Onychomycosis: The Nail Infection That’s Hard to Shake
Fungal nail infections, or onychomycosis, are yet another common affliction in humid environments. The causative agents include dermatophytes, yeasts, and non-dermatophyte molds that invade the nail matrix and surrounding tissue. These infections often begin as superficial discoloration and can progressively compromise nail structure, resulting in unsightly and painful conditions.
The Achilles’ heel of managing onychomycosis is the delayed diagnosis and treatment, which allows the fungus to flourish and establish deeper infections. Consequently, when confronted with a discolored nail, one should consider the underlying possibilities—could this be a harmless condition, or are the destructive fungi accumulating powers to wreak havoc on nail integrity?
Understanding the nuances of this fungal invasion introduces a formidable challenge to healthcare professionals. Diagnostic measures might include microscopic examination, culture tests, and advances in dermatoscopy, although the inherent difficulties in treatment—often requiring prolonged antifungal therapy—pose ongoing challenges for practitioners and patients alike.
The Path to Prevention and Treatment
Equipped with knowledge about the common fungal infections arising from humid climates, it is crucial to analyze preventive strategies and treatment options. Humidity control, meticulous personal hygiene, and prompt medical intervention are indispensable in mitigating the risk of infections and their sequelae.
Environmental modifications can often be implemented to combat humidity at home and in workplace settings. Consider deploying dehumidifiers, aspirating excess moisture, and promoting adequate ventilation—simple yet effective tactics to reduce the likelihood of these fungal nuisances. The challenge lies in harmonizing everyday practices that obliterate fungal habitats while enhancing personal health awareness.
In terms of treatment, a myriad of antifungal agents available both topically and systemically should be employed judiciously. These therapeutic regimens reflect a growing arsenal in the fight against fungal infections, tailored to individual needs and sensitivities. However, professional guidance remains imperative as overuse or misuse can contribute to resistance and exacerbate the problem. Thus, patient education, alongside strategic medical intervention, becomes the linchpin of effective management.
In conclusion, the specter of common fungal infections in humid climates beckons us toward a proactive approach in public health. Knowledge is not merely a weapon of defense but also provokes a reflective challenge regarding our practices, habits, and understanding of environmental interactions with human health. As we strive toward a future where these infections become mere remnants of the past, ongoing education, adaptation, and innovation in healthcare practices are vital. Let this exploration of fungal infections inspire an increased dedication to challenging our assumptions and fortifying our health against nature’s microscopic adversaries.