Fungi are ubiquitous organisms that play an essential role in various ecosystems, yet some of these organisms can pose significant health risks to humans. While many are innocuous or even beneficial, a subset of fungi can lead to infections, allergies, and toxic reactions. This article delves into the world of harmful fungi, focusing on the types that pose threats to human health and how these threats manifest.
Understanding Fungal Biology: The Basics
Before diving into the specifics of harmful fungi, it’s crucial to grasp the complex biology that underlies these organisms. Fungi are neither plants nor animals; they belong to a separate kingdom known as Fungi. They are eukaryotic organisms with a distinct cellular structure that includes a nucleus and membrane-bound organelles. Fungi can reproduce both sexually and asexually, with reproduction often taking place via microscopic spores that are easily disseminated through the air.
The vast majority of fungi are saprophytic, which means they derive nutrients from decomposing organic matter. However, certain fungi shift their lifestyle towards parasitism, living on or within a host, leading to various opportunistic infections. This transition often occurs when the host’s immune system is compromised or when environmental conditions are favorable for fungal proliferation.
The Major Culprits: Pathogenic Fungi
Several fungal species are notorious for their ability to cause diseases. These pathogens can be classified into three main categories: dermatophytes, yeasts, and molds. Each category represents different lifestyle habits and mechanisms of infection.
Dermatophytes: The Skin Invaders
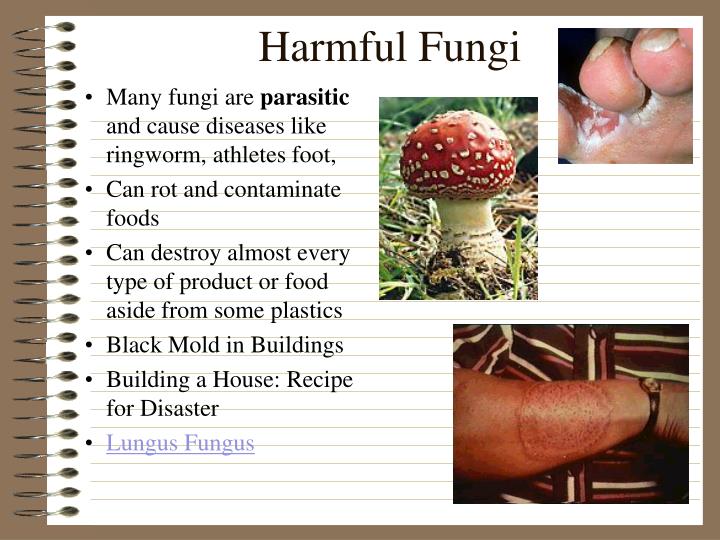
Dermatophytes are a group of fungi that primarily target the skin, hair, and nails. They cause a range of superficial infections, commonly referred to as tinea (ringworm), which can present on various body parts, including the scalp (tinea capitis), body (tinea corporis), and feet (tinea pedis, also known as athlete’s foot).
Exposure to dermatophytes typically occurs in damp environments, such as locker rooms or public pools, where the fungus can thrive. Once established, dermatophytes invade keratin-rich tissues, leading to symptoms such as itching, redness, and flaking. In severe cases, these infections can result in secondary bacterial infections due to intense scratching or skin barrier disruption.
Yeasts: The Opportunistic Pathogens
Yeasts, particularly those from the genus Candida, exemplify opportunistic pathogens that can exploit weakened immune systems. Candida species are ubiquitous inhabitants of human mucosal surfaces, often present in the mouth, gut, and vaginal flora. However, when there is a disruption of the microbiome or a decline in host immunity—be it due to antibiotics, diabetes, or HIV—these yeasts can proliferate uncontrollably.
The most common manifestation of Candida overgrowth is candidiasis, which can range from oral thrush (white patches in the mouth) to vaginal yeast infections. In immunocompromised patients, particularly those hospitalized or undergoing aggressive treatments, invasive candidiasis can occur. This severe condition can lead to bloodstream infections and organ dysfunction, necessitating immediate medical intervention.
Molds: The Lurking Threats
Molds, such as Aspergillus and Mucor species, are another significant class of harmful fungi. These filamentous fungi predominantly affect individuals with pre-existing conditions, particularly those with weakened immune systems or chronic lung diseases.
Aspergillus fumigatus is perhaps the most clinically relevant species. It can be found in soil, compost heaps, and decaying vegetation. Inhalation of its airborne spores can give rise to aspergillosis—a spectrum of diseases from allergic reactions to severe invasive infections. Symptoms may range from a persistent cough, wheezing, and fever to life-threatening pneumonia.
Mucormycosis, caused by molds in the order Mucorales, is another grave condition that can rapidly progress in immunocompromised individuals. It typically presents with sinus and respiratory symptoms but can disseminate to the brain, leading to severe neurological complications.
Environmental Triggers: Increasing Risks
In recent years, environmental changes have escalated the prevalence of harmful fungi. Global warming can expand the geographical range of certain species, allowing pathogens to thrive in previously inhospitable climates. Increasing humidity and the proliferation of mold in urban structures due to inadequate ventilation further augment exposure risks.
Moreover, our reliance on broad-spectrum antibiotics has inadvertently contributed to fungal resistance. Disruption of normal microbial flora allows opportunistic fungi, particularly yeasts, to flourish. As public health concerns mount in relation to antibiotic stewardship, there is an equal need to prioritize the management of fungal infections.
Prevention and Management: Staying Safe
Awareness and proactive measures are paramount in preventing fungal infections. Strategies include practicing good hygiene, maintaining a clean living environment, and managing underlying health conditions effectively.
In general, individuals should keep skin dry and clean, especially in areas prone to moisture accumulation. Wearing breathable clothing and shoes can reduce the risk of dermatophyte infections, particularly during athletic activities.
In settings vulnerable to fungal infections, such as healthcare facilities, stringent infection control practices must be enforced. This includes regular cleaning, proper ventilation, and the use of air filtration systems to minimize the presence of airborne fungal spores.
Treatment options vary based on the type and severity of the fungal infection. Over-the-counter antifungal creams can effectively manage superficial dermatophyte infections, while oral antifungals may be necessary for more extensive cases. In the case of serious infections, intravenous antifungal medications may be required.
Conclusion: Awareness is Key
As we continue to navigate our lives intertwined with fungi, an understanding of the harmful types that can affect us becomes crucial. From dermatophytes to molds, the potential threats are diverse and pervasive.
By fostering awareness, practicing preventative measures, and advocating for responsible health practices, society can mitigate the risks associated with these pathogens. A proactive approach not only safeguards individual health but also contributes to the broader collective well-being, ensuring that the invisible world of fungi does not turn into a visible challenge for humanity.