Fungi are ubiquitous organisms present in virtually every habitat on Earth, demonstrating a remarkable capacity for adaptability and evolution. Certain types of fungi have evolved to exploit the human host, resulting in a spectrum of clinical presentations ranging from superficial infections to life-threatening systemic diseases. Understanding the various types of fungi that cause infections is essential for the effective management and treatment of fungal diseases. This article delineates the major categories of pathogenic fungi, the infections they cause, their pathophysiology, and the clinical implications for affected individuals.
Mycoses, the medical term for fungal infections, can be broadly categorized based on the depth of tissue involvement: superficial, cutaneous, subcutaneous, and systemic mycoses. Each category encompasses distinct fungal pathogens with unique characteristics and pathogenic mechanisms.
Superficial Mycoses
Superficial mycoses are primarily limited to the outermost layers of the skin and hair, generally causing minimal inflammatory responses. These infections often manifest as cosmetic concerns rather than significant health threats.
Tinea Versicolor, caused by the yeast Malassezia, is a prevalent condition characterized by the hypo- or hyperpigmentation of skin patches, particularly in humid climates. The yeast, which is part of the skin’s microbiota, can proliferate abnormally under certain conditions, leading to alterations in melanin production.
Another common superficial fungal infection is Pityriasis Capitis, often known as dandruff, attributed to an overgrowth of Malassezia. While it is fundamental in the aetiology of seborrheic dermatitis, its treatment primarily involves antifungal shampoos or topical agents aimed at reducing the yeast’s population on the scalp.
Though superficial infections may not compromise systemic health, they can have profound psychological impacts due to their visible manifestations and chronicity. This highlights the necessity for effective therapeutic strategies to mitigate their occurrence.
Cutaneous Mycoses
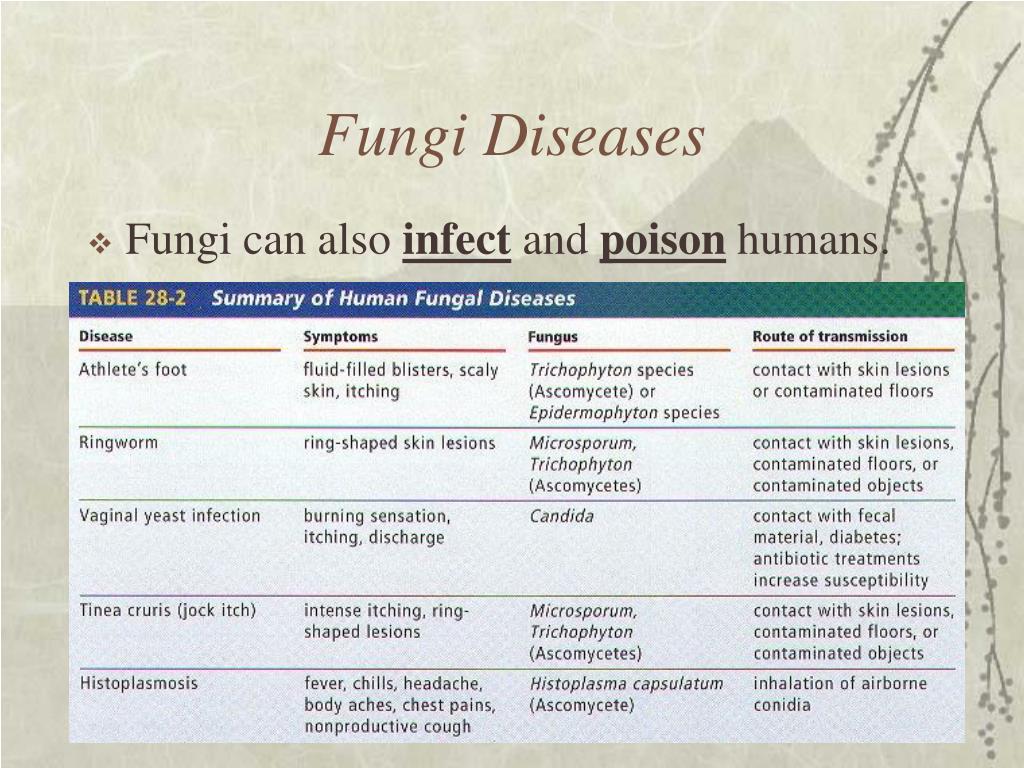
The group of cutaneous mycoses encompasses infections that affect the keratinized layer of skin, hair, and nails. Known as dermatophytes, these organisms, including Trichophyton, Epidermophyton, and Microsporum, thrive in keratin-rich environments and are responsible for several common conditions.
Ringworm, or tinea corporis, is one of the most recognized dermatophyte infections, presenting with erythematous, annular plaques with a raised border and central clearing. The infection is highly contagious, often transmitted through direct contact or indirectly via contaminated surfaces.
Tinea pedis, also known as athlete’s foot, is another prevalent dermatophyte infection that primarily affects the interdigital spaces of the feet. It can progress to extensive skin peeling, cracking, and secondary bacterial infections if left untreated. The use of antifungal agents, both topical and systemic, plays a crucial role in managing these infections.
Nail infections, or onychomycosis, are predominantly caused by dermatophytes but can also result from non-dermatophyte molds and yeasts, such as Candida species. These infections are notoriously difficult to treat and often necessitate prolonged antifungal therapy, coupled with possible surgical intervention for severe cases.
Subcutaneous Mycoses
Subcutaneous mycoses result from the inoculation of fungi into deeper layers of skin and subcutaneous tissue, often through minor traumatic injuries. Fungi responsible for these infections commonly coexist in the environment, particularly in soil or decaying organic material.
Fonsecaea, a genus of dematiaceous (dark-walled) fungi, is implicated in chromoblastomycosis, a chronic fungal infection characterized by cauliflower-like skin lesions. This condition is more prevalent in tropical and subtropical regions, posing challenges for both diagnosis and treatment. Surgical excision, systemic antifungal therapy, and adjunctive therapies, such as cryotherapy, may be required for successful management.
Sporothrix schenckii is the causative agent of sporotrichosis, often referred to as “rose gardener’s disease” due to its association with handling thorny plants. Its clinical presentation can vary from localized skin lesions to disseminated disease in immunocompromised patients. Antifungal treatment is usually effective; however, cases may necessitate a multi-modal approach, especially in chronic manifestations.
Systemic Mycoses
Systemic mycoses are the most severe forms of fungal infections, often resulting from the inhalation of fungal spores. These can lead to disseminated infections that severely compromise the host’s integrity, especially in immunocompromised individuals.
Histoplasmosis, caused by Histoplasma capsulatum, arises from the inhalation of spores found in bird and bat droppings. It often manifests as a pulmonary infection, but can disseminate, affecting organs such as the liver and spleen. The management of histoplasmosis typically involves antifungal therapy, with severe cases requiring hospitalization and adjunctive treatments.
Candidiasis arises from an overgrowth of Candida species, particularly Candida albicans, which can inhabit mucosal surfaces and skin. While often a commensal organism, it can cause opportunistic infections in immunocompromised patients, manifesting as oral thrush, esophagitis, or systemic infections. The treatment of candidiasis may involve topical or systemic antifungal agents, depending on the sites of infection and severity.
Cryptococcosis, caused by Cryptococcus neoformans, is an opportunistic infection associated predominantly with immunosuppressed individuals, such as those with HIV/AIDS. The pulmonary and central nervous system are often involved, with meningoencephalitis as a common, life-threatening manifestation. Early diagnosis and prompt antifungal treatment drastically improve patient outcomes.
The Need for Vigilance and Future Directions
With the rising incidence of fungal infections, particularly in immunocompromised populations, vigilance in diagnosis and treatment is paramount. The advent of antifungal resistance among certain pathogens complicates management strategies and calls for ongoing research into novel antifungal agents and therapeutic regimens.
Furthermore, public health initiatives aimed at educating communities about preventive measures, especially in environments predisposed to fungal exposure, could mitigate the risks associated with these infections. Early recognition and prompt treatment cannot be overemphasized in reducing the morbidity and mortality associated with fungal diseases.
In conclusion, a nuanced understanding of the various types of fungi that cause infections can enhance the clinical approach to managing mycoses. By recognizing the key characteristics and treatment modalities associated with superficial, cutaneous, subcutaneous, and systemic mycoses, medical professionals can better navigate the complexities of fungal infections, contributing to improved patient outcomes and overall public health. The interplay between fungi and hosts necessitates not only therapeutic interventions but also preventative strategies to curtail the impact of these opportunistic pathogens.